A nutrition plan to ease digestion
If you suffer from digestive issues such as irritable bowel syndrome (IBS), you may be a candidate for low-FODMAP Eating. As part of this healing diet, certain foods are restricted, which produce a fermentation process in the gut. For some people, this process triggers a sensitivity. By following a low-FODMAP eating plan, you may be able to avoid any resulting gastrointestinal distress.
low-FODMAP is an acronym: FODMAP stands for the names of molecules in food that are frequently poorly digested. These molecules are fermentable oligosaccharides, disaccharides, monosaccharides and polyols – all carbohydrates. Wheat, milk, soft cheeses, onions, garlic, legumes, honey are examples of foods that share these properties.
The basics of low-FODMAP eating
This eating plan was originally created for IBS sufferers by researchers in Australia. An estimated 10 to 15 percent of adults suffer from IBS. Using these specialized nutrition guidelines, people have found relief from the severe gas, diarrhea, constipation and pain associated with IBS. There is evidence based on a short-term University of Michigan study that patients with IBS do experience relief using the low-FODMAP method.
People with other conditions causing ongoing, severe digestive symptoms can consider a low-FODMAP eating plan for possible relief. For instance, this diet may reduce the symptoms for people suffering from diverticulitis, an intestinal disorder where inflamed or infected pouches form on the colon.
There are three stages to the low-FODMAP eating plan: restriction, reintroduction and personalization. Restriction involves a three to eight-week restriction of all FODMAP foods. During reintroduction, you determine which types of FODMAP foods you can tolerate. The last step, personalization, is where you put your new, slightly restricted eating plan into place. This allows for the greatest possible symptom relief, while eating a wide variety of foods and receiving all essential nutrients.
Seeking professional guidance
Many people who begin the low-FODMAP eating plan do so with a nutritionist or doctor’s guidance.
Sheila Crowe of University of California at San Francisco supports the low FODMAP diet. She sees its growing popularity among doctors and patients, but believes people should enlist the support of a professional before beginning it.
“Any time you have to have a dietary intervention, you have to have education, have to have worked with a dietitian,” she said.
A nutritionist will assist you in sticking to the rigorous, though short-term, restriction part of the plan. They can also help you come up with meal plans and address any other health issues that could affect the dietary guidelines. Many nutritionists who specialize in certain dietary plans have made their own low-FODMAP dietary guides. Together, you can shape the program to your specific needs.
A nutritionist will also assist with the tricky business of stages two and three of the plan. At these stages, they can help you tinker with your diet, introducing small amounts of FODMAP foods one-by-one. After you see how your gut tolerates them, together you will determine a more feasible, long-term dietary plan.
Part of the benefit of using a nutritionist is that for those people who don’t actually need this plan, it could have a negative effect on their health. That’s partly because the foods excluded by low-FODMAP dieting are prebiotics – fibers that encourage healthy gut bacteria growth. To ensure a person is getting enough prebiotics for a balanced gut, it’s essential that anyone on this restrictive plan have some guidance.
That being said, the low-FODMAP eating plan is a good option for anyone with IBS to consider. It’s also an option for those unhappy with severe gastrointestinal issues that don’t respond to stress-management or other dietary interventions. Enlisting professional help is a great idea with a diet this specific. That way you can ensure you aren’t depriving your body of much-needed nutrition. By carefully introducing this new dietary plan, you may be able to reduce or completely remove your painful abdominal symptoms.
Those sidelined by gastrointestinal pain and discomfort of conditions can sometimes find some relief in mindful, stress-management strategies. Because the mind-gut connection is so strong, it may be healing to add mindful meditation as a treatment for IBS or IBS-like symptoms, alongside a program like the low-FODMAP.
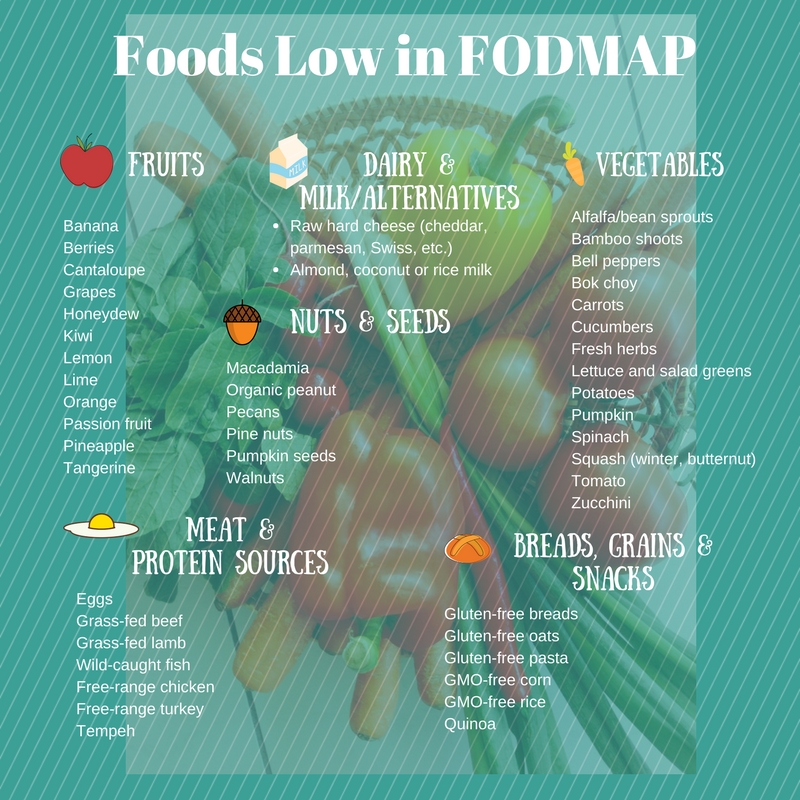
Foods low in FODMAPs include: