Writing about visiting her mother who has Alzheimer’s disease, Priscilla Warner observes, “I try not to go with expectations, but that’s hard, since… I want my visits to go well. But it’s hard to define ‘well’ when my mother doesn’t know who I am.” Watching her mother deteriorate over time, Warner sometimes forgets herself and asks (then immediately regrets), “What are you thinking?” Her mom replies, “It’s hard to tell.”
Writing about visiting her mother who has Alzheimer’s disease, Priscilla Warner observes, “I try not to go with expectations, but that’s hard, since… I want my visits to go well. But it’s hard to define ‘well’ when my mother doesn’t know who I am.” Watching her mother deteriorate over time, Warner sometimes forgets herself and asks (then immediately regrets), “What are you thinking?” Her mom replies, “It’s hard to tell.”
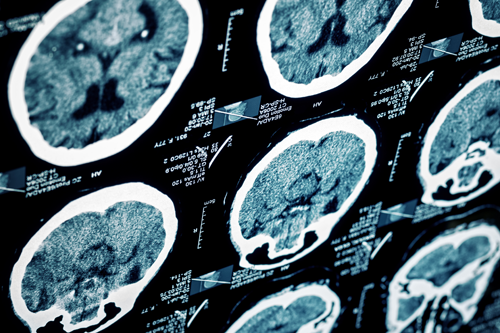
“In the past, studies and treatments have placed the spotlight on brains that contain the plaques and tangles of Alzheimer’s sufferers. There’s just one problem: Having these physical signs doesn’t mean you’ll develop the disease.”
I understand Priscilla’s wish for visits to go well and then finding yourself tripped up over the most basic conversational elements. I’ve written about wondering whether an orchid could have saved my grandmother’s brain. Research shows that gastrodin, an orchid root extract, may have powers to prevent Alzheimer’s disease. And while gastrodin remains in the alternative and holistic health market, some interesting shifts are occurring in the mainstream that may upend all we thought we knew about Alzheimer’s and, possibly, pave the way for a more substantial, curative process.
The History of Alzheimer’s Theory
In 1906 Alois Alzheimer identified the cause of Alzheimer’s disease as the accumulation of the sticky, plaque-forming protein beta amyloid. According to Alzheimer (and still believed by the majority of present-day researchers), beta amyloid plaque strangles healthy cells, which degenerates the brain and leads to symptoms such as reduced memory, thinking, and reasoning skills. According to data from the American Alzheimer’s Association, more than 5 million adults 65 years or older currently have Alzheimer’s disease. Staggeringly, that number is predicted to rise to 16 million by 2050. With the current total cost of Alzheimer’s patient care topping $150 billion in the U.S. annually, the need for a cure is enormous.
Well over a century after Alzheimer’s theory took root, more than 100 drugs have been developed targeting beta amyloid—and every single one of them has failed. The research marketplace has now expanded from studies focusing on the efficacy of beta amyloid targeters to trying to determine whether the format of the studies themselves is flawed. A big question is whether the drugs are being administered too late. Specifically, scientists are wondering how results might change if medication were given to patients who evidence increased amyloid in their brains but do not yet show symptoms.
Researchers at Harvard Medical School are currently recruiting 1,000 symptom-free people whose brains show amyloid pathology. They’ll be tested with a new imaging agent (developed by pharmaceutical company Eli Lilly & Co.) that binds to beta amyloid in the brain. The agent is radioactive, which means a simple magnetic resonance imaging (MRI) test will show the degree to which the protein has accumulated. The new study will administer Eli Lilly’s most recent beta amyloid–targeting medication and then gauge the results. This is the first study engaging late-onset (zero-symptom) participants; if it fails, it will add another crushing blow to Alzheimer’s original theory.
Overturning the Theory
Across the Atlantic, Claude Wischick, a chair in mental health at the University of Aberdeen in Scotland, isn’t afraid to rock the Alzheimer’s research boat. The founder of a Singapore-based pharmaceutical company (TauRx), he’s one of several scientists pulling back the curtain on accepted Alzheimer’s disease ideology. Wischik muses, “It’s extraordinary that in the face of [the] failed trials, the claims for amyloid remain exactly the same, as though there haven’t been any failures. There’s been no fundamental revision of the thinking.”
Stepping into the void, Wischick has a theory of his own. He believes that beta amyloid is only one of many elements that challenge the brain’s cellular garbage-disposal process. Another component is tau, a protein used by cells to maintain open channels through which they receive nutrients. When tau functions inappropriately, it forms clumps that prevent cells from getting the food they require. And here’s what’s really disturbing: When tau goes rogue in one area of the brain, it creates a domino effect. Over time, an increasing amount of tau functions improperly until patients devolve into Alzheimer’s disease.
“In another example of developing a new approach to Alzheimer’s research, the Harvard team working with REST focused not on what could be seen in terms of possible brain destruction but instead on the brain’s inborn strengths.”
In the 1990s many studies actually proved that the degeneration of tau correlates more directly to Alzheimer’s disease than does beta amyloid. That would seem to have been enough to shift the focus from one protein to the other. Insiders say, however, that funding tau research meets resistance from grant decision makers devoted to amyloid theory. Wischick responded to this predicament by developing his own study through TauRx. Studies with TRX-015, a compound that targets sickness-generating tau, showed that a significant number of participants scored 5.5 points better on a 70-point cognitive test—and maintained those results more than a year later—versus participants taking a placebo. While these results offer hope, they have not yet been published in a peer-reviewed journal. Regardless, Mike Williams, editor of the Journal of Biophysiology, remains optimistic. “We’ve still got so many other findings in the wings,” he says. “If any of these got prioritized and funded to the extent of amyloid, we might be a lot closer to getting a drug than we are now.”
Looking Toward a New Theory
At the same time that old ideas are being questioned, new research indicates that the brain itself may be able to fend off Alzheimer’s disease. According to recently published material in Nature, Harvard Medical School researchers discovered that a protein called repressor element 1-silencing transcription factor (REST) controls protective mechanisms in the brain. The new theory: Failure of this system could lead to Alzheimer’s disease.
In the past, studies and treatments have placed the spotlight on brains that contain the plaques and tangles of Alzheimer’s sufferers. There’s just one problem: Having these physical signs doesn’t mean you’ll develop the disease. In another example of developing a new approach to Alzheimer’s research, the Harvard team working with REST focused not on what could be seen in terms of possible brain destruction but instead on the brain’s inborn strengths.
When a brain ages in healthy ways, REST protects cells from the harm of destructive proteins and “oxidative stress,” a process that is much like the work of antioxidants. It also prevents the death of brain cells by acting on specific genes. Even people who are 90+ years old have shown high levels of REST. In fact, raised levels of REST appeared in Alzheimer’s-susceptible areas of the brain. Conversely, study results revealed that participants with mild cognitive decline had lower levels of REST and that those with the least amount had Alzheimer’s. This led the Harvard researchers to conclude that individuals with high levels of REST may have inborn defenses against dementia.
Of the results, an author of the study, Bruce Yankner, M.D., Ph.D., professor of genetics and neurology at Harvard Medical School, says, “There is a lot of evidence to suggest that major lifestyle modifications that protect the heart will also protect the brain—such as a healthy Mediterranean-type diet and frequent exercise…good mental health may also be beneficial.”
Yankner’s idea may be the most promising of all. As a culture, we have a long way to go in moving away from lifestyle habits ingrained from childhood and toward healthy nutrition and consistent exercise, plus stress reduction and improved mental health. But the news that these elements may fend off Alzheimer’s disease (among other illnesses) suggests the possibility that it matters less whether you’re on the side of beta amyloid, tau, or any other agents and more that you’re on the side of what you can do personally to help increase your brain health with the small daily choices you can elect to make.
Read more about the Alzheimer’s disease and how to prevent it by clicking here
Post Disclaimer
This content is for informational purposes only and does not constitute medical advice. Please consult a healthcare professional for any medical concerns.